AI-Powered Plaque Analysis: Transforming Heart Disease Detection at UVA Health
Cardiovascular disease remains the leading cause of death worldwide, but a breakthrough technology being studied at UVA Health is reshaping our understanding of the problem and how we approach treating it. By applying artificial intelligence (AI) to coronary CT angiography (CCTA), UVA Health researchers are uncovering critical details about arterial plaque composition, providing a new dimension of insight into heart disease risk.
Todd Villines, MD, a cardiologist and heart disease researcher at UVA Health, is helping lead this transformative work. His team’s focus is on identifying what arterial plaque is composed of — because it’s not just about how much plaque exists in the coronary arteries, but what’s inside that plaque also matters.
“We’ve known that plaque burden is the strongest predictor of future heart attacks,” Villines explains. “But what we’ve now learned is that the composition of that plaque is also key. Some types of plaque are far more likely to rupture and cause serious cardiac events.”
AI Plaque Analysis Fills in Heart Disease Risk Details
Traditional imaging techniques require manual evaluation, a sometimes time-consuming and imprecise task, especially when trying to quantify total or non-calcified plaque volumes. This is where AI comes in.
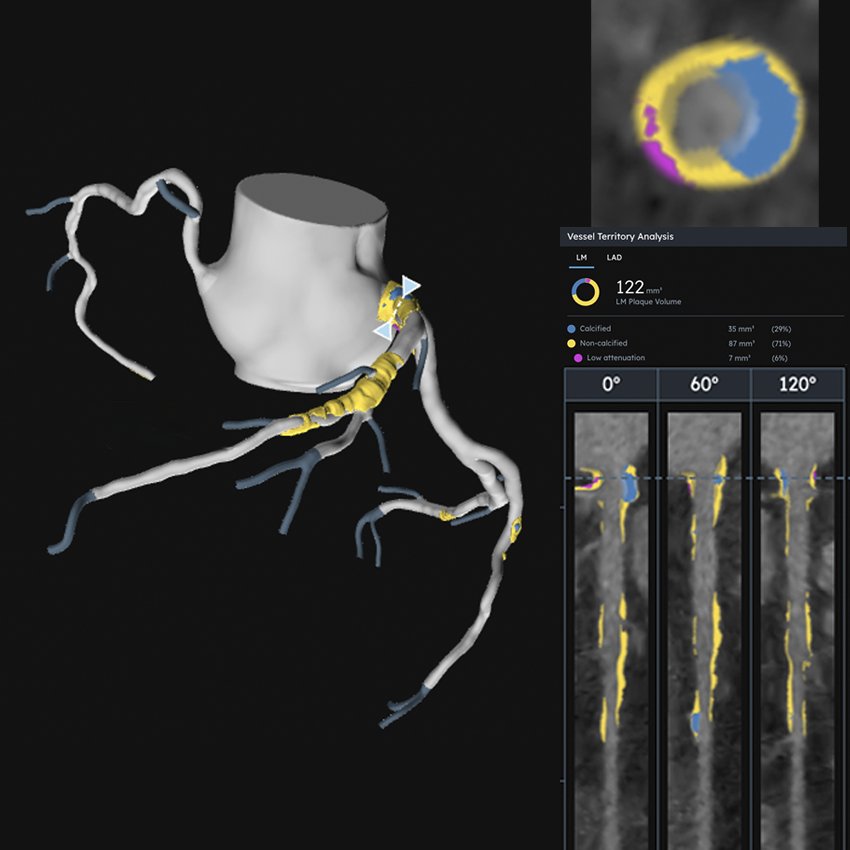
AI can process CCTA images quickly and consistently, quantifying the volume of plaque but also identifying the presence and amount of high-risk plaque. Low-attenuation, lipid-rich, or positively remodeled plaques are especially concerning, and AI can flag these with far greater speed and reproducibility than human reviewers.
“Coronary CT angiography (CCTA) identifies several important characteristics of coronary artery plaque that include how much it is narrowing the lumen of the artery, called stenosis, the amount of calcification, proportion of plaque that is non-calcified, and plaques that have high-risk features, as described above. Using this information, CCTA provides a comprehensive assessment of coronary risk based on the amount of total and high-risk coronary plaque, degree of stenosis (narrowing), and the type of plaque (high risk or not),” says Villines.
“AI allows us to quantify plaque volume and composition in a way that’s simply not feasible manually. Most AI algorithms use the density or brightness (Hounsfield units, HU) of plaque to identify areas of high lipid (cholesterol) content, such as <30 HU, non-calcified plaque, and calcified plaque. The challenge with this approach is that it requires high-quality CCTA images. Furthermore, the brightness of plaque can vary according to technical factors, such as how the CCTA scan was performed, what type of scanner was used, etc. It also helps reduce variability between readers, ensuring more consistent and reliable results. This technology may also allow us, for the first time, to non-invasively measure whether a patient’s coronary artery disease is progressing (getting worse) or stabilized or even getting better in response to their current treatments in cases where patients have undergone two CCTA examinations. Measuring plaque progression or its change to medical therapies is not practical without AI-enabled plaque software," Villines notes.
The implications for patient care are profound. Both U.S. and international guidelines already recognize CCTA as a first-line test for evaluating patients with chest pain. The addition of AI analysis means patients and their physicians may gain a clearer understanding of their heart disease risk, even if no significant artery blockage is present.
In December 2025, the American College of Cardiology released a a report spotlighting this research.
Spotting High-Risk Patients Earlier for Better Intervention
This discovery opens the door to earlier intervention. If a scan reveals plaque whose volume or composition puts the patient at higher risk for an adverse heart event, they can begin lifestyle changes or medical therapy before a heart attack occurs.
“Our goal is proactive care,” Villines says. “We now have safe, effective medications that lower cholesterol, reduce inflammation, and improve outcomes. But you have to know there’s a problem to treat it.”
While still in early stages, AI-powered plaque analysis is rapidly gaining traction. UVA Health is among the pioneers exploring not only the clinical impact, but also the cost-effectiveness and broader implementation of the technology. The Centers for Medicare and Medicaid Services (CMS) may begin reimbursing AI-based plaque analysis in 2026, further accelerating adoption.
“Cost is currently the biggest barrier,” Villines admits. “But with more evidence showing improved outcomes and more efficient care, we believe this technology will become a standard part of cardiac evaluation. We are excited to offer this tool to patients at UVA Health in the near future.”
AI Analysis Promise: Better Outcomes for Cardiac Patients
For Villines, the work is personal. Because several of his family members developed early heart disease, he pursued cardiac CT research to give patients a better alternative to traditional stress tests and vague risk scores.
“I’ve seen firsthand how devastating heart disease can be,” he says. “Being able to provide precise, personalized insight into someone’s heart health and then take action before something happens is incredibly powerful.”
By pushing the boundaries of medical science at the intersection of AI and clinical care, UVA Health is committed to delivering smarter, more effective care. Villines says, “Further work is currently ongoing to better standardize our methods for plaque quantification so that patients and their doctors can be even better informed as to how they should be treated following a CCTA scan.”


